Calling the hospital billing office might be one of the most stressful consumer experiences people are still forced to endure. By then, they’ve waited weeks for a bill that’s higher than expected, doesn’t make sense, or isn’t something they can afford. And now, they’re stuck on the phone, explaining their financial situation to a complete stranger just to figure out what to do next.
On the other end of that call? Someone who likely has answers but is barely keeping their head above water. All day, they’re digging through complex systems, piecing together account details, and trying to resolve issues as quickly as possible. Patients are frustrated, the workload never lets up, and the pressure is high. Is it any wonder hospital billing offices see such high turnover?
Sound familiar? There’s another way.
What’s different now? AI can actually help this time.
Yes, there’s endless hype around AI in healthcare. Go to any industry conference in 2025, and the only thing you’ll hear more than “agentic AI” is people joking that it’s the only thing they heard.
But, jokes aside, GenerativeAI (GenAI) and large language models (LLMs) offer genuinely powerful solutions—particularly in an industry so dependent on labor. With hospitals spending approximately 60% of their expenses on labor costs, AI applications that address operational inefficiencies represent one of the highest-impact opportunities in healthcare today.
Of course, AI isn’t a silver bullet on its own. As Nworah Ayogu, MD, of Thrive Capital points out:
““AI should not be the selling point. The conversation should be about how it uniquely and distinctly solves your problem. Full stop.”
Here’s our take: billing call centers represent an ideal problem space for this technology—high-cost operations where the right tools can reduce workload, improve efficiency, and create a substantially better patient experience. But before providers dive into AI investments, they need to understand exactly what they’re trying to solve.
That’s why we analyzed 4,000 billing calls at a large health system in 2024.1 While every patient population is different, the patterns we discovered likely mirror what’s happening at a high level in your environment and offer immediately actionable insights.
So why are patients calling?
As a company that provides digital patient payment solutions, we’ve often heard that some patients will always call in—no matter how simple the online experience is. While there’s probably some truth to that, they’re likely not calling just to make a payment.
Instead, most patients—by far—are reaching out with questions about their bills, insurance coverage, and financial assistance. It’s not exactly surprising in an era of high deductibles and complex plan designs, with healthcare costs on everyone’s minds.
Top 10 reasons patients call the hospital billing office
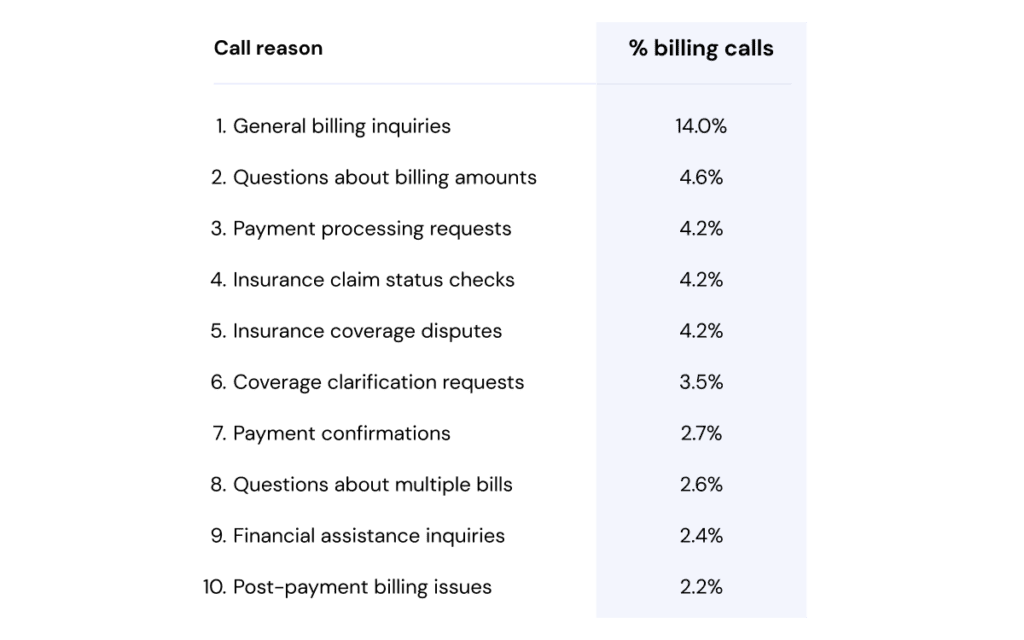
But the real insight? These aren’t always simple questions with easy answers. They’re often navigation challenges, spanning multiple stakeholders. When a patient asks, “Why is my bill so high?” or “Is this covered by insurance?” they could be unknowingly initiating a complex dance involving third-party payers, HSA administrators, or eligibility and enrollment vendors, among other stakeholders.
This fragmentation could be a hidden driver behind long call times and repeat callbacks. Call center agents often function as human routers between disconnected systems—translating complicated information while also being the calm voice helping a parent understand their child’s Emergency Department charges or advocating for financial assistance.
And this is precisely where AI with the right integrations can really shine. By connecting to multiple data sources—e.g., payers, HSA banks, financial assistance programs—AI can synthesize information that normally requires human navigation through siloed systems. These insights can be delivered through voice assistants, agent support tools, or directly in payment portals—helping prevent calls before they happen or resolving them faster when they do.
The challenge isn’t just the questions
It’s also the variability. We found that a seemingly simple billing question can actually be one of 71 different inquiry types, stemming from 61 different root cause groups, and requiring one or more interventions spanning 99 different resolution categories.
To make this more concrete, let’s unpack “Why is my bill so high?” What seems like a straightforward question actually branches into multiple scenarios that require very different responses:
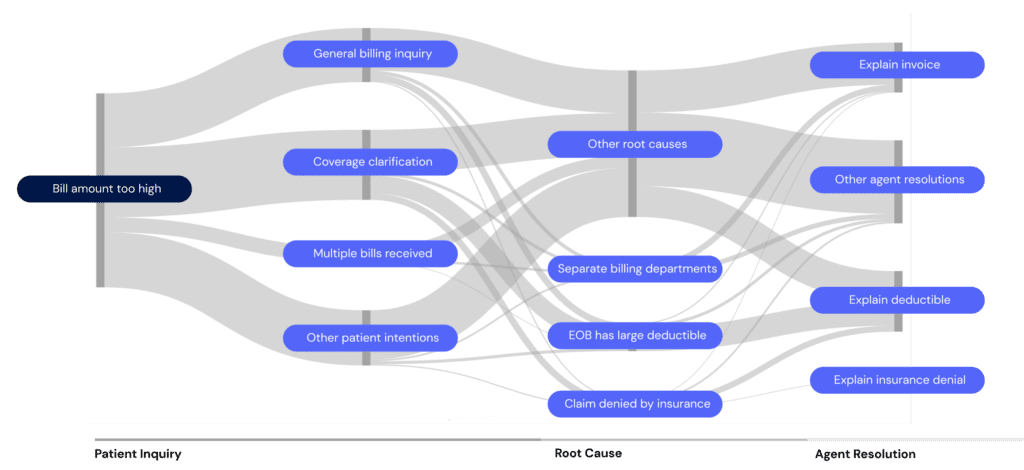
In other words, agents must invest significant time to learn hundreds of potential customer service pathways, recognize subtle patterns across multiple scenarios, and maintain quality in resolutions. And this complexity has real operational implications:
- Long onboarding times: Extensive training for new agents before they can handle complex cases independently.
- Knowledge retention challenges: With so many possible scenarios, even experienced agents can encounter edge cases they haven’t seen before.
- High cognitive load: Agents must maintain patient rapport while mentally sorting through diagnosis paths and fussing with systems.
Perhaps unsurprisingly, this also makes a strong case for AI-powered automation. By identifying common pathways and high-volume interaction patterns, providers can target specific scenarios where AI can enhance or replace manual processes while, importantly, maintaining a human-like touch.
How? Well, unlike the rigid “press 2 for billing” phone trees of the past, conversational AI feels like talking to a knowledgeable, empathetic person (just try Kora, our AI voice agent, to hear the difference). Patients can speak naturally about their issues and the AI system understands, responds contextually, and provides personalized answers—especially when it integrates with third-party resources.
Which calls can AI actually handle?
Our analysis shows that today’s AI technology could handle up to nearly a third of billing calls autonomously. For patients seeking clarity about their financial responsibility, this means getting answers right when they need them.
- The simplest of calls are direct requests where patients know exactly what they need—like an itemized statement or payment confirmation.
- Others are more complex but still predictable interactions. These typically start with questions about bills or insurance benefits and often involve third parties. While they require multiple steps of investigation and explanation, they follow clear patterns that AI can handle.
In total, that’s 30% of call volume that could potentially be automated right now based on Cedar’s 2025 AI roadmap. But the true impact goes far beyond this initial assessment. To illustrate this potential, we modeled how AI adoption could fundamentally change the economics of billing call centers.
Illustrative call center FTE costs: traditional vs. AI-powered improvements2
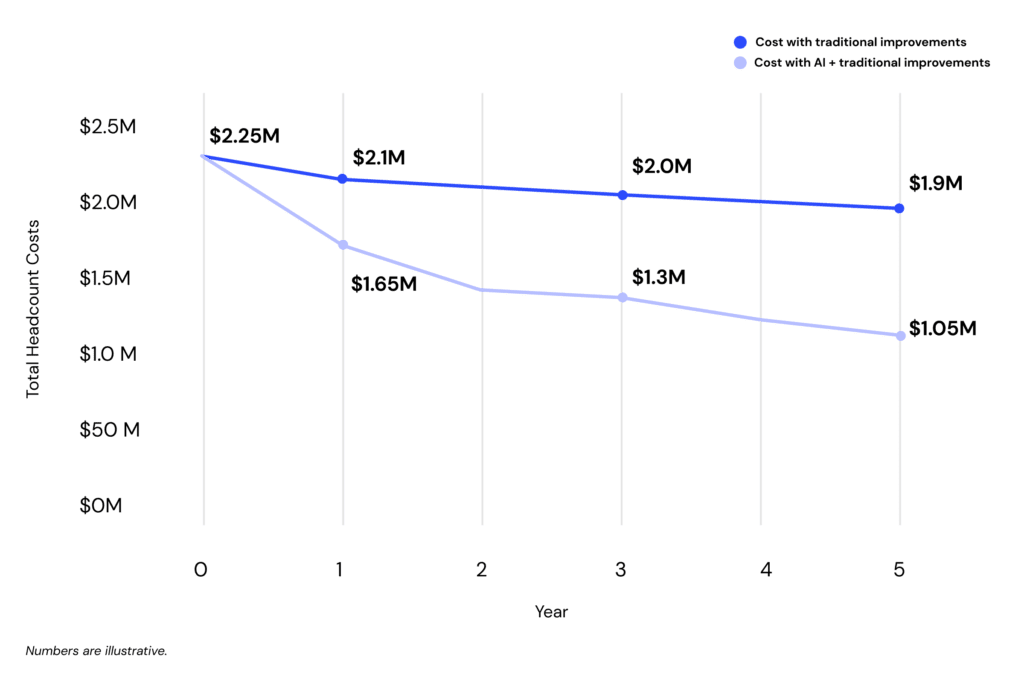
The model shows AI dramatically outperforming traditional improvements over five years. Starting with the same baseline (50,000 monthly calls, 45 FTEs), the model shows AI can drive step-change efficiency—conservatively saving over $3.5 million in staffing costs with constant call volume by year five. Imagine not having to backfill every open position, while keeping your top performers focused on the complex cases where they can make the biggest difference.
Bottom line
If you’ve been burned by technology promises before, skepticism about AI in healthcare is understandable. But unlike many hyped solutions, we believe patient billing support automation offers clear, measurable benefits today—and it will only get better.
For patients, that means getting accurate information without the frustration of hold times and transfers. For agents, it’s less time wrestling with disconnected systems and more time using their empathy and judgement where it matters most. And for providers, lower costs, greater efficiency, and a differentiated patient financial experience.
Want to dig deeper? Here’s where to start:
- Meet Kora, the AI voice agent built to handle the nuance of patient billing support
- Hear from Montefiore’s George Stein on separating hype from reality in healthcare AI
- Let’s get technical with a peek behind the curtain at how we’re building with LLMs
Ben Kraus is Director, Content Marketing at Cedar