For too long, healthcare has placed the burden of patient billing on providers alone. This series explores how Cedar’s ecosystem partners—providers, payers, HSA banks, and other stakeholders—are working together to deliver a transformational financial experience.
When patients leave the hospital, the financial experience can get chaotic.
They may be forced to interact with a whole set of stakeholders beyond the health system. The result: a mess of paperwork and disconnected systems that lead to frustration and confusion, missed payments, administrative waste, and poor outcomes for everyone involved.
Take health benefit accounts, like health savings accounts (HSA) and flexible spending accounts (FSA). If a patient wants to check their balance before paying a bill in their provider’s portal, they must access a separate bank portal with separate login credentials. And that’s if they remember that they have a health benefit account.
This friction inevitably leads to some patients missing out on opportunities to save on care. They may think twice about paying bills out of pocket. They may even implicate their payer for insufficient coverage.
Highmark and Allegheny Health Network recognized this gap in the experience and knew the only way to fix it was through an aligned approach.
Leveraging the power of connection
Payers typically have partnerships with HSA banks and providers own the patient billing process. Why not combine the two to create a seamless and integrated experience for patients?
This is precisely what Highmark and Allegheny Health Network did. Using Cedar’s Payer Intelligence Layer, the payer-provider pair uniquely incorporated health benefit accounts into patient bills.
Specifically, when Highmark members receive care at Allegheny Health Network, they now conveniently view real-time HSA and FSA balances in the same place where they manage their bills. Furthermore, outbound billing reminders encourage these patients to use available funds for payment.
Connected HSAs/FSAs influence payment behavior
After only six months, Highmark and Allegheny Health Network have seen remarkable results with the Payer Intelligence Layer.
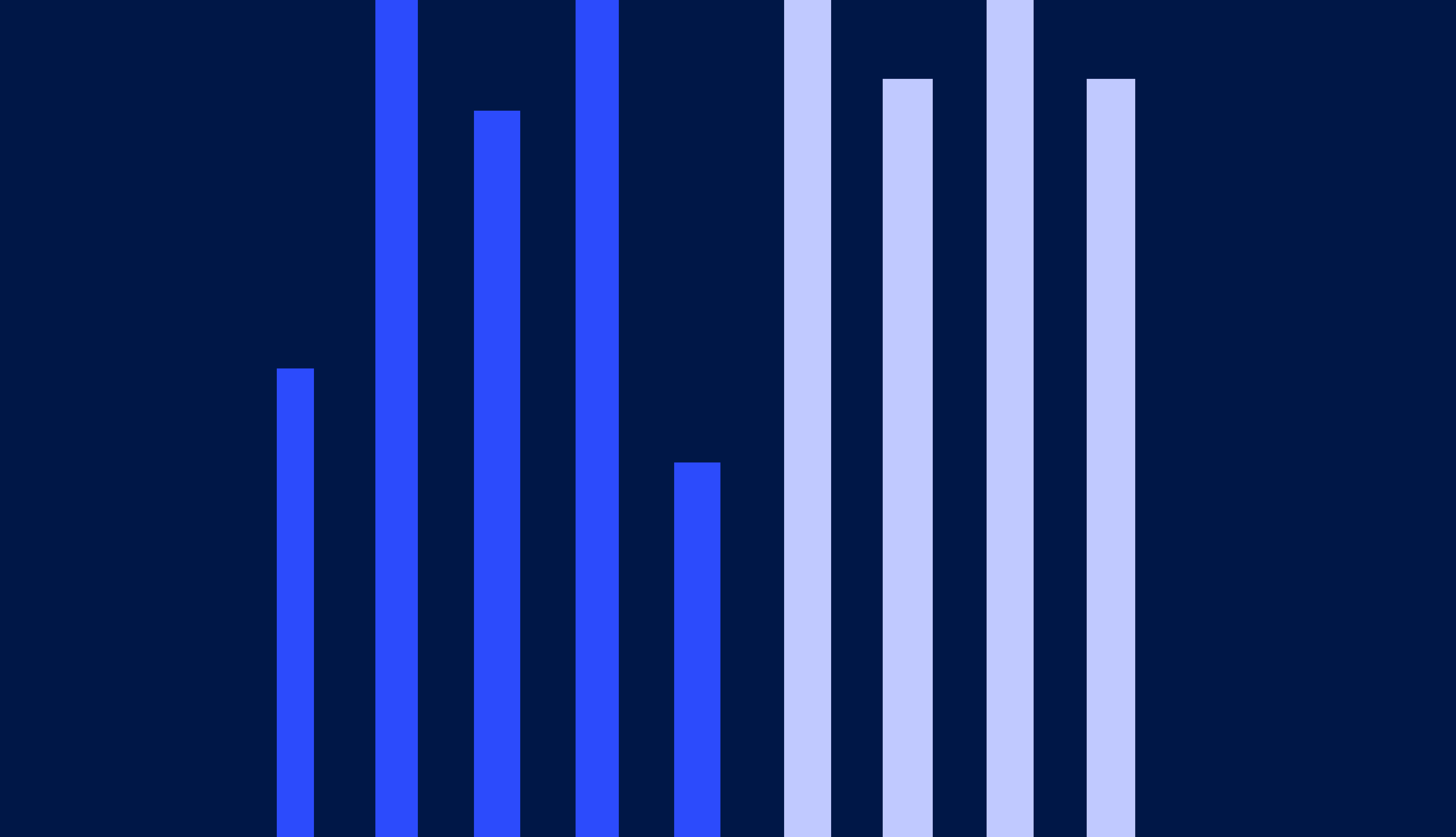
The reminders and easy access to health benefit account balances have led to a 33% increase in HSA and FSA utilization. This dramatic behavior change demonstrates that patients value the seamless and consolidated experience, closing the gap for a more optimized healthcare spending pattern.
This also leads to more payments, as it’s easier for patients to spend money already allocated for medical expenses. By just how much? Stay tuned for the impact on the collection rate in a future post.
Perhaps most importantly, patients appreciate the added convenience. Instead of fussing with multiple portals or cumbersome reimbursement processes, they now have all the information at their fingertips to make better payment decisions.
“I love the option of clicking a button to view my HSA balance before paying my bill using it. Before I would have to go to a separate site and log in, etc. But this new feature makes it very convenient and easy.”
Want to dig deeper? Hear James Rohrbaugh, Chief Financial Officer of Allegheny Health Network, discuss his organization’s strategy for ecosystem connectivity. Plus, keep an eye out for upcoming posts that tell more of the Highmark and Allegheny Health Network story by signing up for our newsletter below.
Ben Kraus is a Content Strategy Manager at Cedar