For too long, healthcare has placed the burden of patient billing on providers alone. This series explores how Cedar’s ecosystem partners—providers, payers, HSA banks, and other stakeholders—are working together to deliver a transformational financial experience.
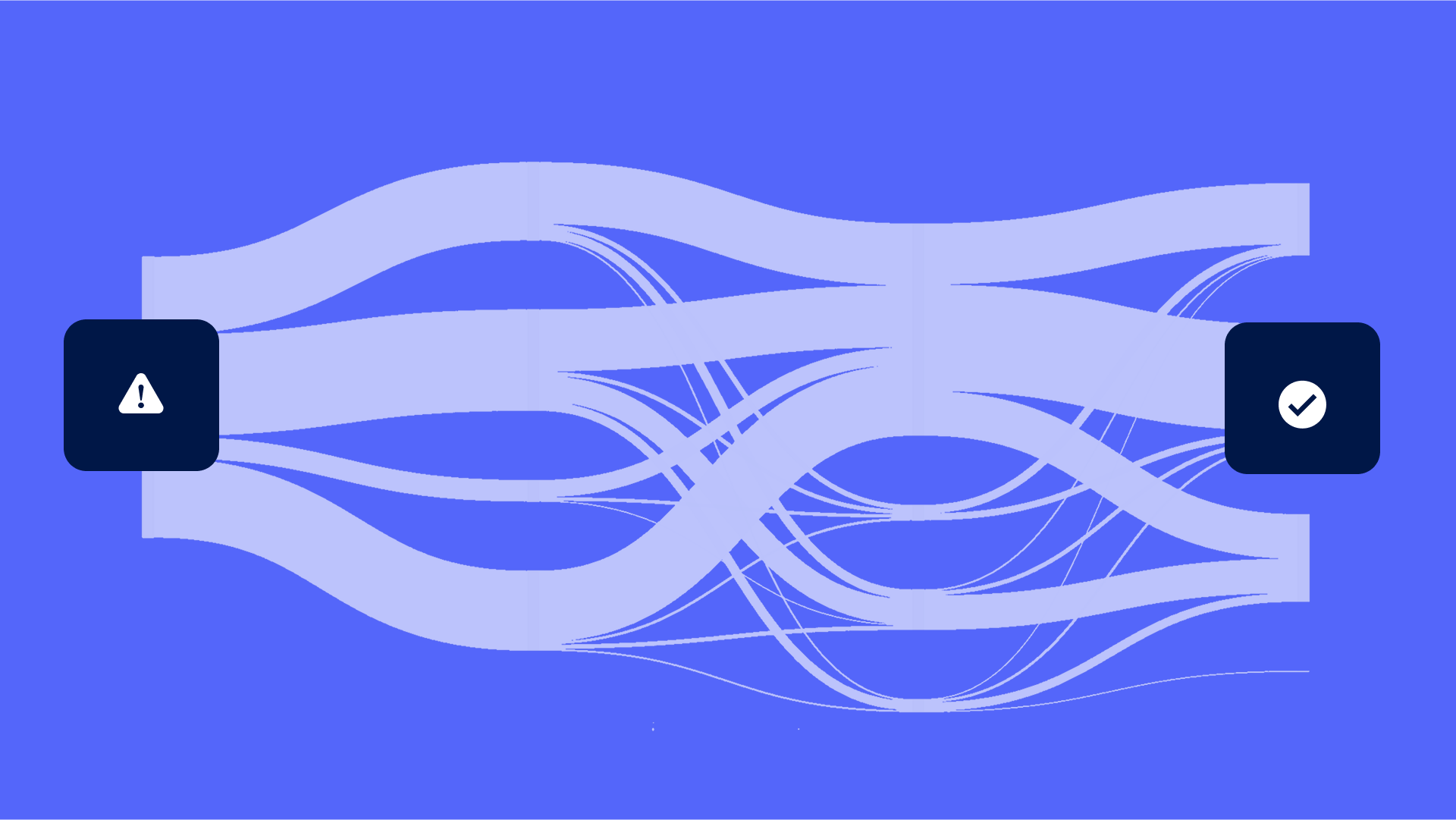
Despite provider-led efforts to make the patient billing process timely, simple, and convenient, patients still experience confusion and frustration. The problem? Patients are typically not only interacting with the provider but are also navigating a complex web of touch points involving multiple stakeholders.
For instance, when insured patients receive a bill, they have to engage with both their provider and payer. The provider informs them about their financial responsibility and collects payments, while the payer communicates coverage information and administers the health plan. These two sets of processes occur independently, leaving patients caught in the middle.
Consequently, patients often question the accuracy of their bills. In the best-case scenario, this leads to payment delays and costly customer service inquiries. At worst, unpaid bills and customer dissatisfaction.
Recognizing these challenges, Highmark and Allegheny Health Network knew they needed to take a bolder, more coordinated approach to simplify patient billing.
One provider, one payer, one experience
When Cedar asked patients about what providers and payers could do to improve the billing experience, they suggested something that sounds simple but is hard to do: offer a single source of truth for managing healthcare payments.
This aligned perfectly with Highmark and Allegheny Health Network’s Living Health model. The strategy employs a blended approach that connects payers, providers, community organizations, and tech innovators to build a better healthcare ecosystem for everyone.
Using Cedar’s Payer Intelligence Layer, Highmark and Allegheny Health Network worked together to deliver a uniquely integrated patient billing experience. Specifically, balances due are now verified by the payer on patient bills and real-time deductible status is on clear display in the provider’s payment portal.
Additionally, patients can view real-time health savings account (HSA) and flexible spending account (FSA) balances in the same place where they manage their bills.
Payer-provider alignment builds trust and drives efficiency
After six months, Highmark and Allegheny Health Network have seen a 13.5% reduction in patients reviewing itemized bills prior to payment, thanks to the coordinated approach. This suggests patients trust that their insurance benefits have been accurately applied to their bills without the need for further investigation.
As a result, patients are less likely to call in with simple, repetitive questions about billing and insurance. There has been an 11% decrease in call transfers from the provider’s payment portal, freeing the customer service team to handle more complex inquiries.
“What I’ve been struck by is how responsive patients are to seeing the Highmark logo on their billing statement and having it come from Allegheny Health Network,” said James Rohrbaugh, Chief Financial Officer of Allegheny Health Network. “It takes away the fragmentation that we have between the payer and the provider.”
Reduced friction and increased trust have also driven patient payments. Stay tuned for the Payer Intelligence Layer’s impact on the collection rate by signing up for Cedar’s newsletter below.
For more information about how Highmark and Allegheny Health Network are collaborating to transform the patient financial experience, check out these resources:
Ben Kraus is a Content Strategy Manager at Cedar