Cedar Solutions for Payers
Remove the systemic friction that confuses members, frustrates providers and distracts from the true mission of healthcare.
Boost member satisfaction, establish aligned goals with your provider network and reduce administrative costs with Cedar’s Payer Intelligence Layer.
Highmark Health’s primary goal is for customers to feel happy, satisfied, and confident in the information they’re receiving. We want them to return to Allegheny Health Network or continue their coverage because we work together to make it so simple and easy.Vice President of Customer & Clinician Experience Solutions, Highmark
I’ve been impressed by how much Cedar’s payer integration affects patient engagement. I have my provider saying this is good to go. I have my insurance saying it’s good to go. Great, I can pay with confidence.Director of Revenue Cycle Strategic Initiatives and Optimization, Allegheny Health Network
-
Increase member engagement and satisfaction with a single source of financial information
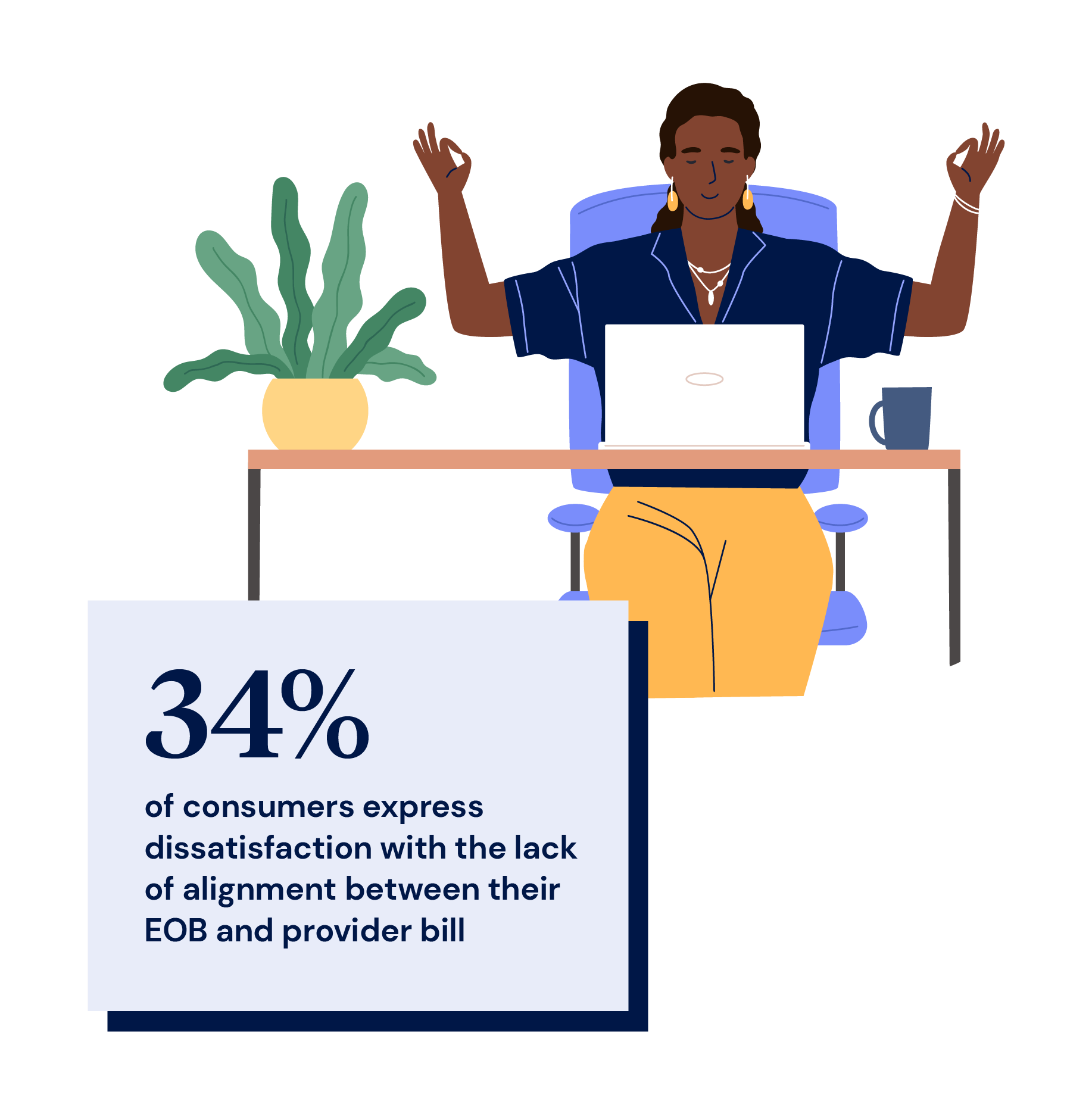
Eliminate confusion caused by conflicting statements with a single, clear presentation of financial responsibility to members.
- Members have clarity of what they owe and to whom
- Member engagement increases as does NPS, STAR ratings and other customer satisfaction metrics
- Accumulators, HSA balances and EOB matching take the guesswork out of the member experience

-
Differentiate your organization by aligning with your provider network.
Provide unprecedented clarity to your members’ experience, generating loyalty and satisfaction for your brand
- Members have unprecedented accessibility, clarity and affordability for their healthcare services
- Align goals with your provider network for productive partnership. Create trust and confidence with common goals
- Provide a superior experience to members, compared to your competition

-
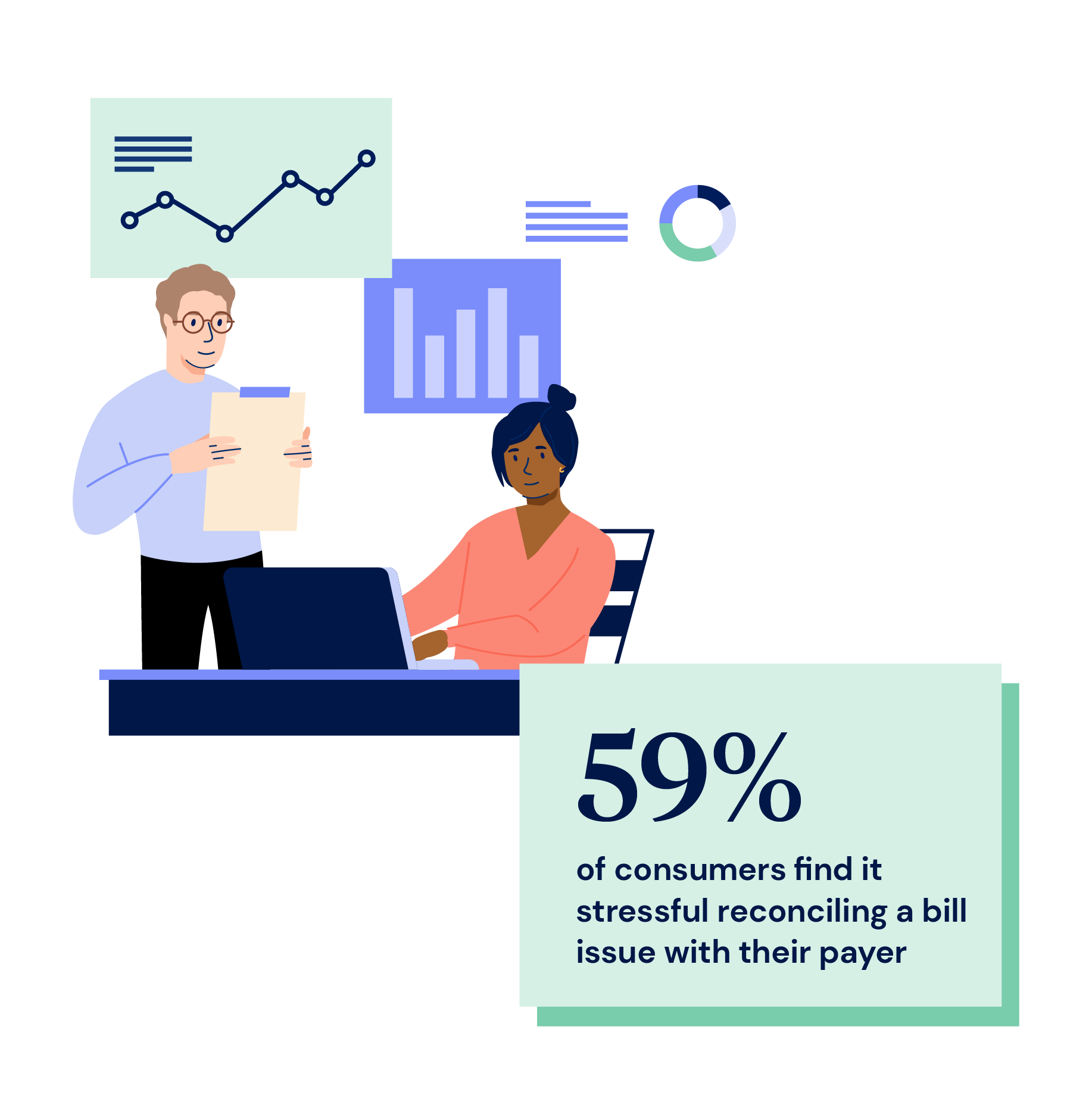
Ease administrative burdens for good
Self-service and engagement dramatically increases when provider bills and EOBs match
- Personalized, clear communications result in reduced member calls to customer service
- Post-service billing and bad debt is reduced when members understand their financial responsibility
- Increased engagement and self-service results when financial responsibility is clearly communicated


Find out more about Cedar
Cedar Pay
Increase patient collections and deliver a superior experience by combining health plan data with patient billing for simplified patient payments.
Resources
Explore Cedar’s library of helpful case studies, research reports and more