The Change Healthcare cyberattack sent shockwaves through U.S. healthcare, grinding critical operations to a halt and severely straining cash flows. While unprecedented in scale, it highlights an all-too-familiar challenge for revenue cycle teams: disruption.
From system outages and file delivery issues to broken reports and new technology deployments, it can feel like an endless game of whack-a-mole. During the scramble to maintain operations, teams risk overlooking one important aspect: the patient financial experience.
At Cedar, we’ve been analyzing the Change Healthcare outage’s effect on patient payments with our clients. Then we thought: why not share our approach more broadly? It applies to other kinds of system failures, and our findings point to clear patient engagement opportunities.
Let’s dive into how to measure and mitigate patient impact during inevitable future disruptions.
IT outages hit differently
When it comes to technology disruptions in healthcare, impact can vary wildly. Your systems, operations, payer mix, and even patient population can all play a role in how hard you’re hit.
Take the Change Healthcare outage, for instance. Some providers found themselves wrestling with delayed cash posting and patient billing due to remit processing issues. Others saw denial rates climb as authorization and verification tools went down. And for those heavily reliant on affected payers? Their cash flow slowed to a crawl.
Crisis mode became the new normal. Many organizations were forced to manually work accounts, deprioritizing other critical tasks. What’s more, providers’ historical collection rates came into play too—those with typically high performance fared better.
Given this variability, how do you pinpoint the patient impact at your organization?
Patient impact indicators to watch
In the wake of the Change Healthcare outage, we collaborated with clients to monitor these key metrics:
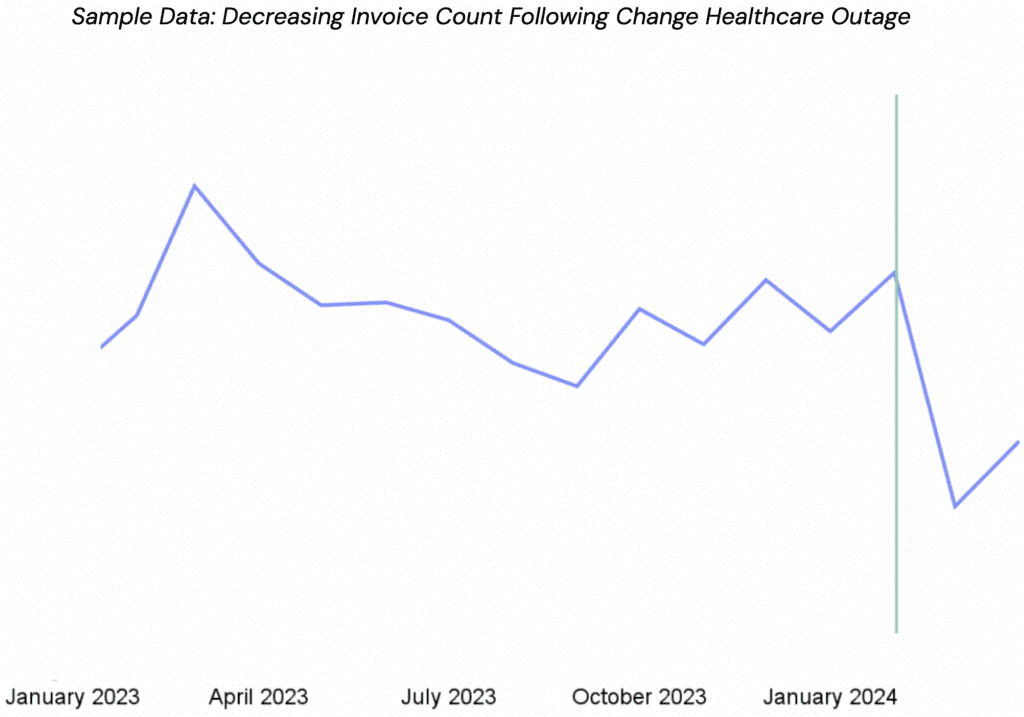
Invoice count and total patient responsibility
If you can’t bill patients in a timely manner, you may observe fluctuations in your invoice count and total patient responsibility. Initially, you might see a decrease in these metrics as claims are held or delayed. Once the issue is resolved, expect a substantial increase as the backlog is processed.
To accurately gauge the impact:
- Compare year-over-year trends for the affected period.
- Examine the decreases during the disruption and the subsequent increases post-resolution.
Factor in typical seasonal fluctuations to isolate the disruption’s true impact.
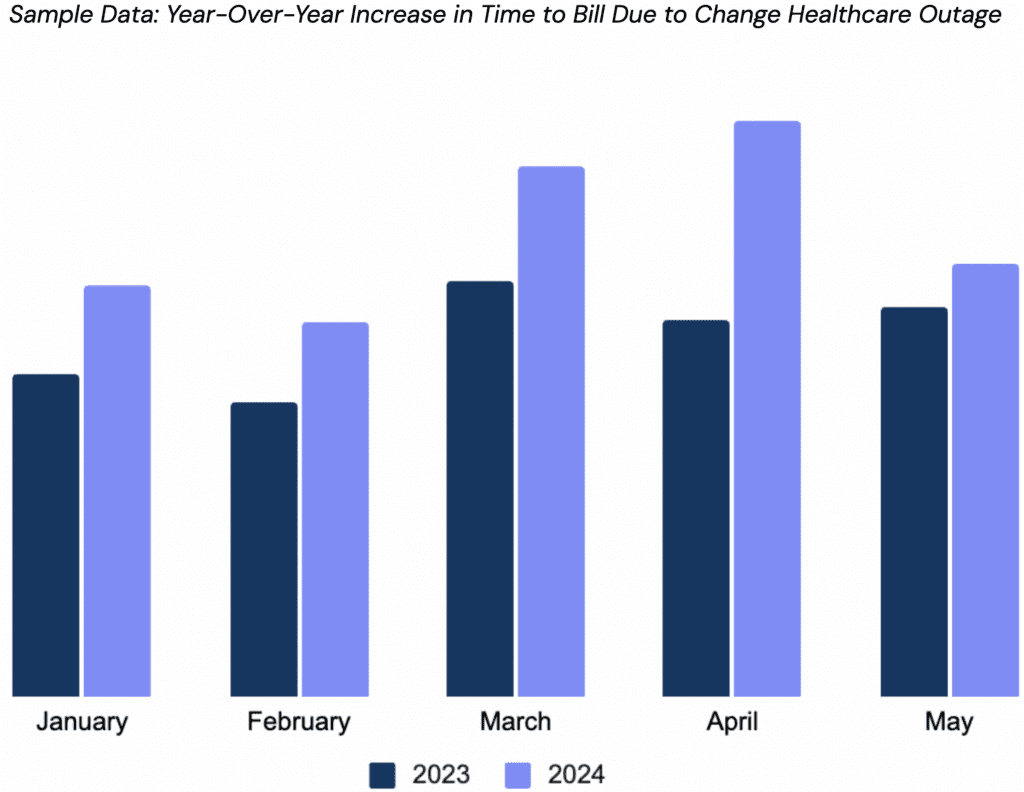
Time to bill
At Cedar, we’ve found a clear link: the longer it takes to send a bill, the lower the collection rates. This makes analyzing time to bill a crucial metric. To assess performance, compare the duration between patient visit dates and billed dates from previous years to the current year.
During the Change Healthcare outage, we observed an increase in days to assign to Cedar in March and April 2024 across our impacted clients. This increase resulted from held claims and the time needed for operational processes to manage the invoice backlog.
Pro tip: Group previous years’ time to bill into aging tiers (e.g., 0-29 days, 30-59 days), and analyze collection rates for each to establish baselines. Compare these to current tiers to quantify an outage’s impact on different billing timeframes.
Collection rate and cash reporting
Cash collections serve as a vital barometer of financial health during any disruption. Specifically, look for deviations from expected trends. The Change Healthcare outage in February and March 2024 provides a stark example: organizations likely saw reduced payments despite March typically being the highest payment month for health systems and physician groups.
Patient satisfaction
Patient satisfaction, while less quantifiable, is equally crucial to monitor during disruptions. Extended delays between service and billing often lead to patient confusion and frustration. Remember, patients are rarely privy to the intricacies of denials, appeals, bill holds, and operational changes that can cause these delays. During any system outage or operational hiccup, these issues can be amplified.
Preparing for the unexpected
Identifying the impact of system disruptions on patients is just one step. The real challenge—and opportunity—lies in how we respond. Drawing insights from the recent Change Healthcare outage, we’ve developed a set of strategies to help you navigate future disruptions.
1. Optimize your patient payment reporting for better insights
You can’t manage what you can’t measure. This makes having the right reporting in place crucial to tracking patient impact indicators.
While many organizations rely on their EHR as the primary source for patient payment reporting, we’ve found that these systems often lack critical out-of-the-box reports. For example, determining patient responsibility frequently requires revenue cycle leaders to run complex SQL queries—a time-consuming and potentially error-prone process.
To address this gap, consider working with your IT team to set up these essential reports internally or partnering with a vendor that can deliver this capability.
2. Embrace digital outreach for faster, more effective billing
In patient billing, every day counts. Relying solely on paper statements can delay the process, potentially exacerbating the impact of a disruption. By leveraging SMS and email notifications, you can get bills into patients’ hands sooner.
Speed, however, is just one benefit. The real power in digital outreach is its ability to drive engagement. Our data shows that if patients don’t engage with their bills within the first 10 days of receiving them, the likelihood of digital engagement drops significantly. This narrow window underscores the importance of timely, effective communication.
Focus on fine-tuning your outreach. Consider when you’re sending messages, which channels you’re using, and what you’re saying. Getting these elements right can increase the chances of patients taking action, even when there’s a system hiccup.
3. Send proactive communications to keep patients in the loop
When billing goes sideways, your patients need to know. Sending out quick, ad hoc messages about known delays isn’t just a good practice—it’s a trust builder. By being upfront, you’re heading off frustration and showing patients you’ve got their back.
Now, take a moment to consider your current patient billing system. Can it respond quickly when it matters most? Many EHR systems, for instance, require IT support for even minor communication changes. This becomes a major roadblock when your technical teams are swamped managing a system outage.
4. Develop contingency plans to prepare your operations
Preparation is your best defense against system outages. Develop clear, actionable downtime contingency plans and ensure your entire team knows them well. Regular training sessions can turn these plans into second nature.
What recent large systems outages have shown is that effective contingency strategies need to go deeper than what many security and compliance programs have established, and should include immediate response procedures, patient communication protocols, and temporary workarounds for critical processes and services. By having these plans ready and your team prepared, you can significantly reduce the patient impact of unexpected disruptions.
The bottom line
Make no mistake: your revenue cycle’s reliance on technology will only grow, and with it, the risk of disruptions. The Change Healthcare outage was just a preview of challenges to come. As we navigate this new reality, it’s crucial to adopt a proactive approach to managing system failures.
It might also be time to rethink your vendor strategy. Look beyond feature grids and vendor questionnaires—seek partners who can help you navigate these tough moments. Because when technology falters, it’s not just your operations at stake—it’s your patients’ trust and financial well-being.
Don’t let the next IT outage catch you off guard. Request a free, in-depth assessment of your patient financial experience, including industry benchmarking, from Cedar today.
Nicole Olszewski is Senior Manager, Value Engineering at Cedar



