Built for patients. Powered by intelligence. Proven in performance.
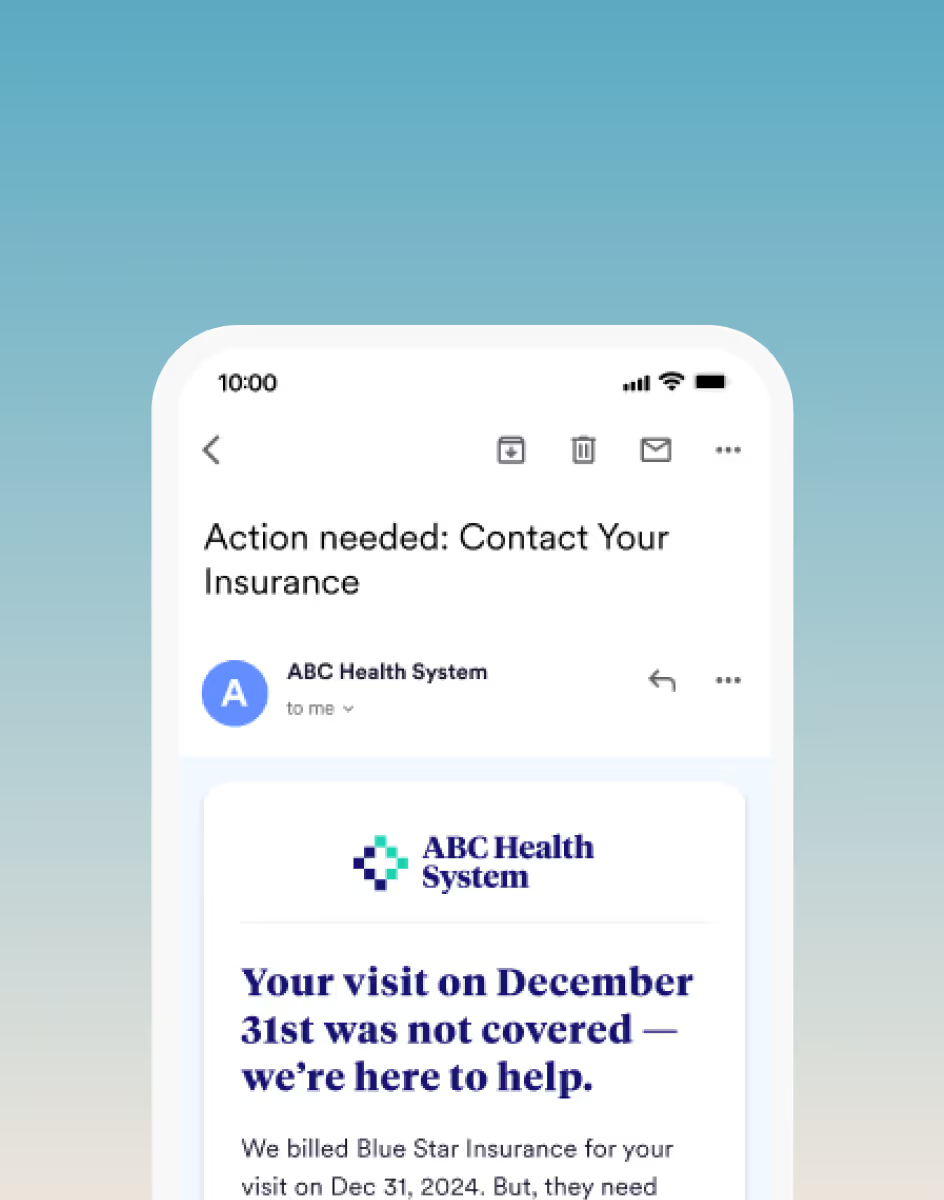
Cedar unifies billing, payments, coverage, and support through one intelligent platform—driving stronger margins for providers and simpler financial experiences for patients.

The financial intelligence healthcare has been waiting for
Cedar Intelligence brings together deep healthcare financial data, advanced learning models, and proven outcomes to create a system that continuously adapts to patients and providers.
Unlike general-purpose AI, Cedar Intelligence is built exclusively for patient financial engagement—understanding the nuances of billing, coverage, payments, and affordability to drive real results: higher collections, lower costs, and stronger patient trust.
It powers Cedar’s ability to personalize interactions, optimize the funnel, and unify channels—from digital payments to Kora, our intelligent voice agent.
Leading providers rely on Cedar
From health systems to physician groups and clinician service agencies, leading providers choose Cedar to transform their patient financial experience.












.svg%201.svg)










Get more from every financial touchpoint
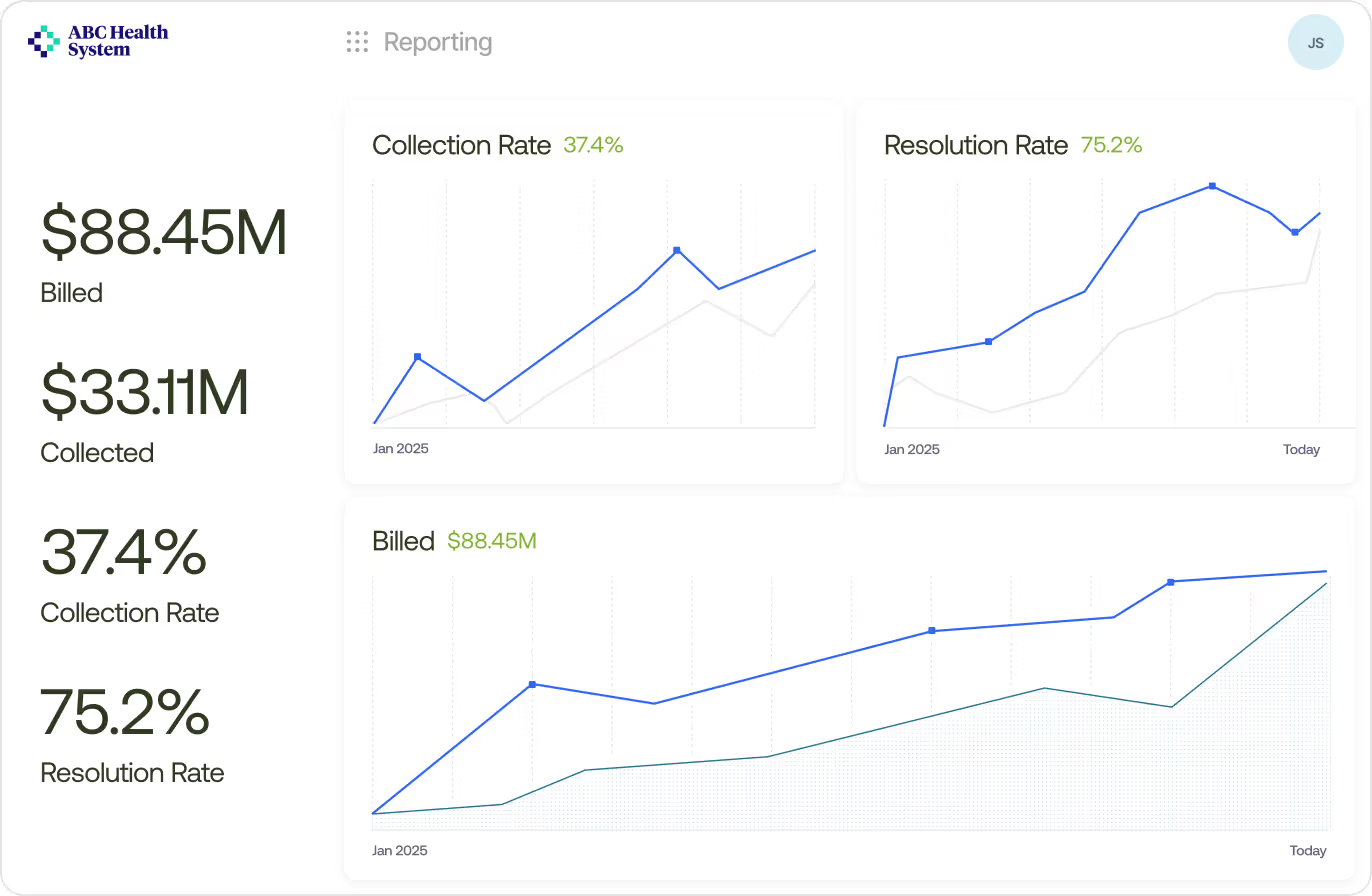
Intelligence that scales. Performance that delivers.
With billions of patient transactions and millions of lives served, Cedar’s data foundation powers better outcomes for every partner we serve.
Patient payment interactions
Patients served
Patient payments processed
The complete patient financial experience platform
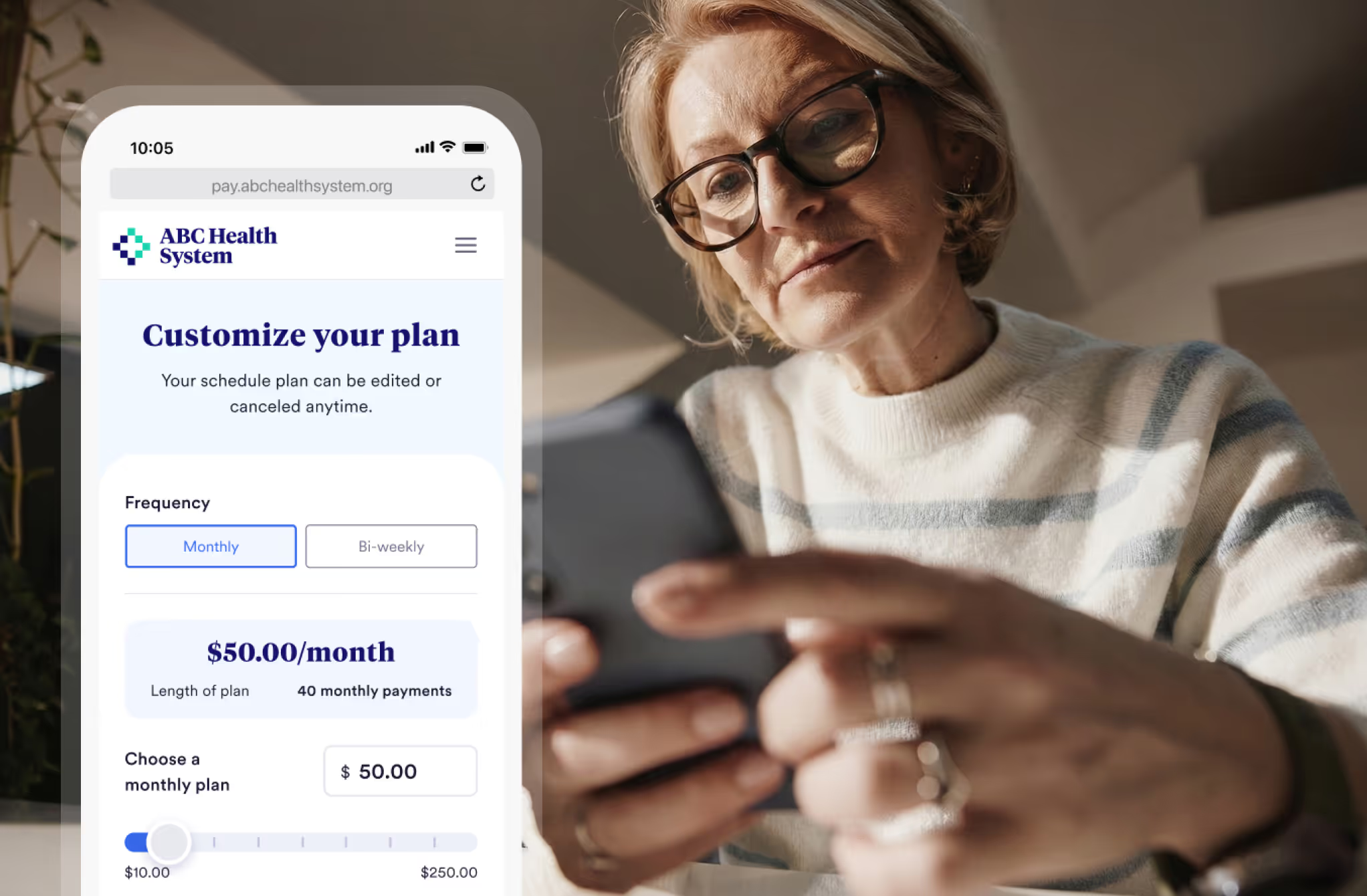
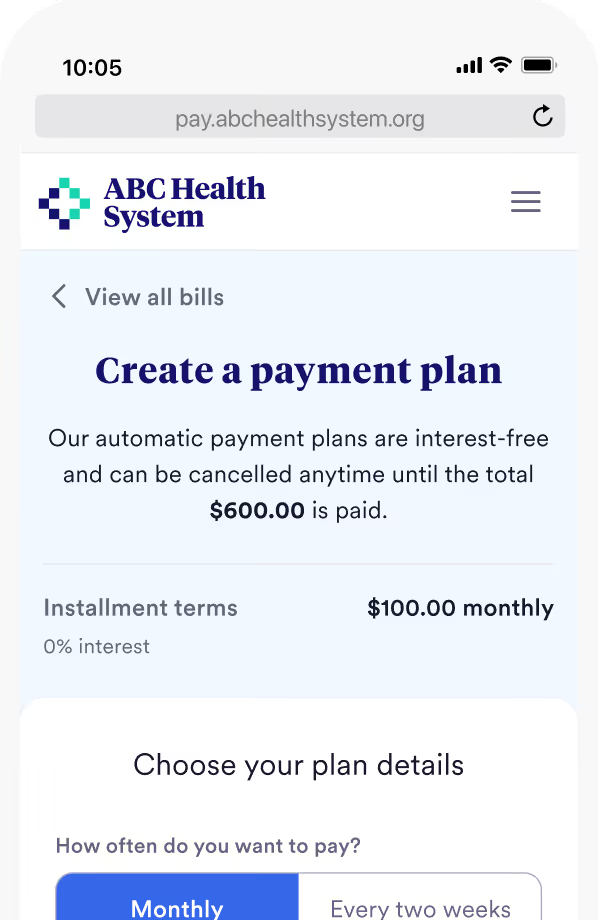
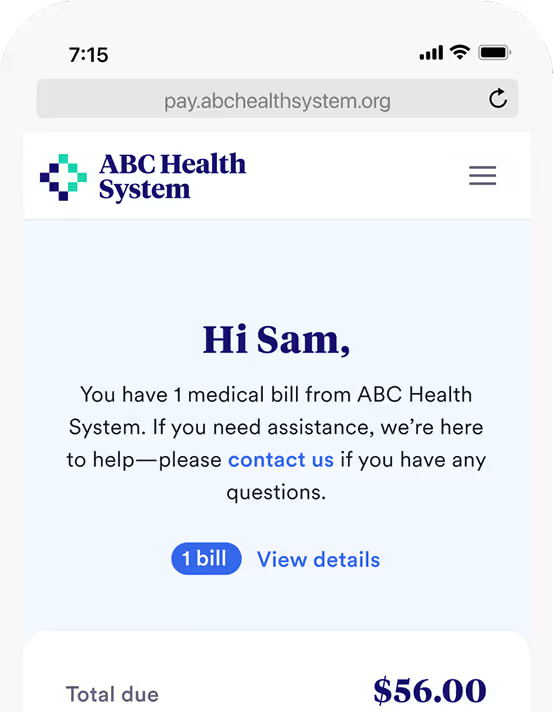
Increase Patient Payments
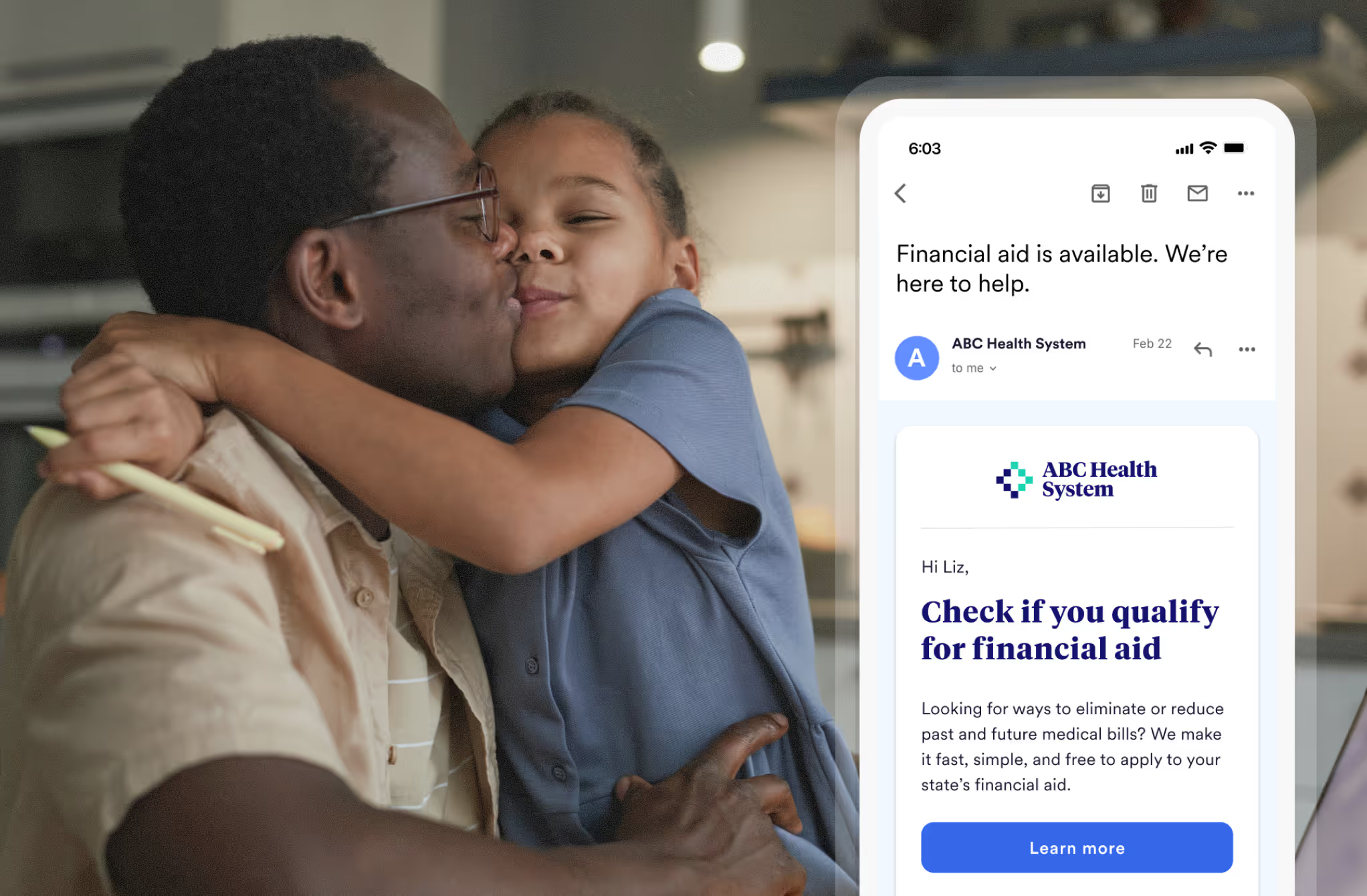
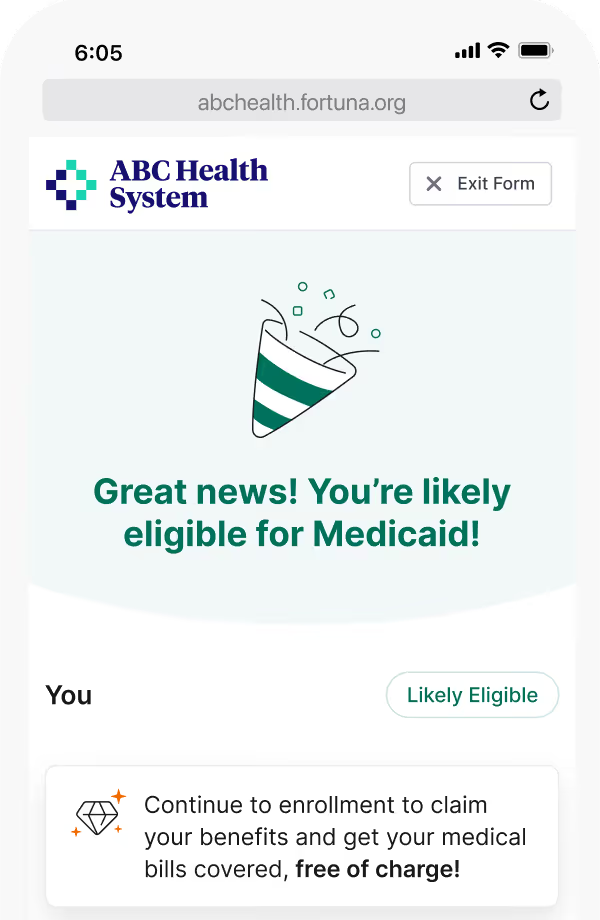
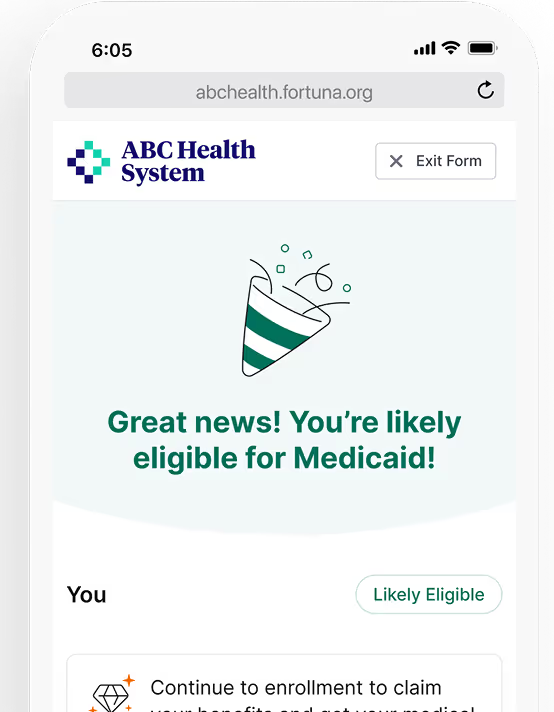
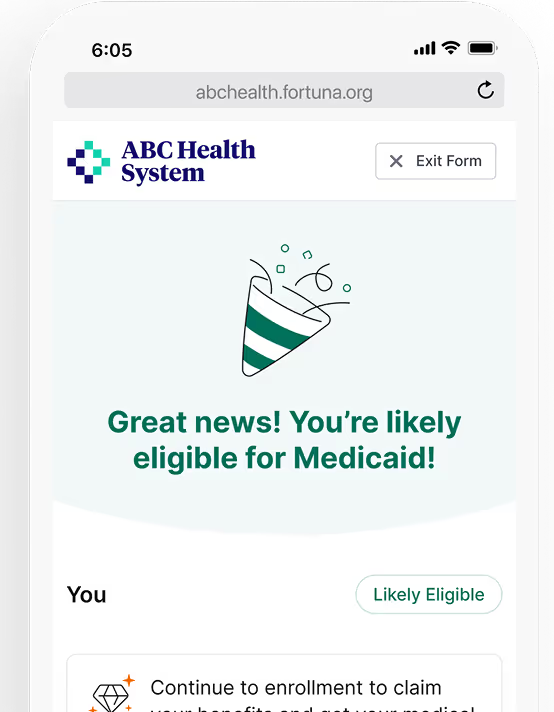
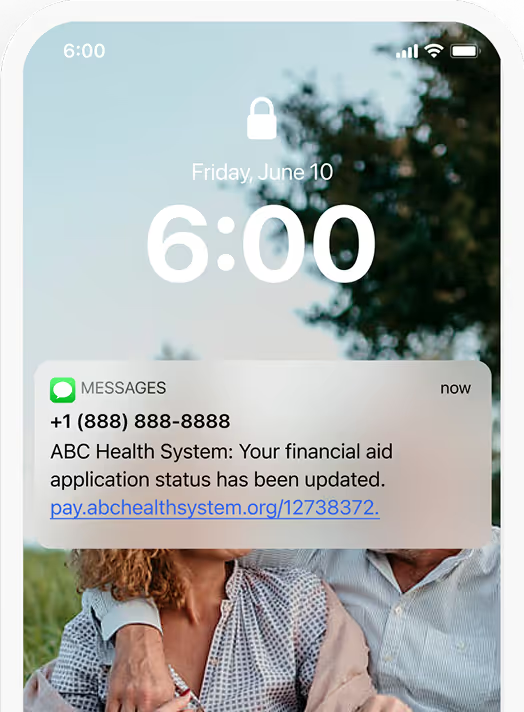
Expand Coverage and Aid
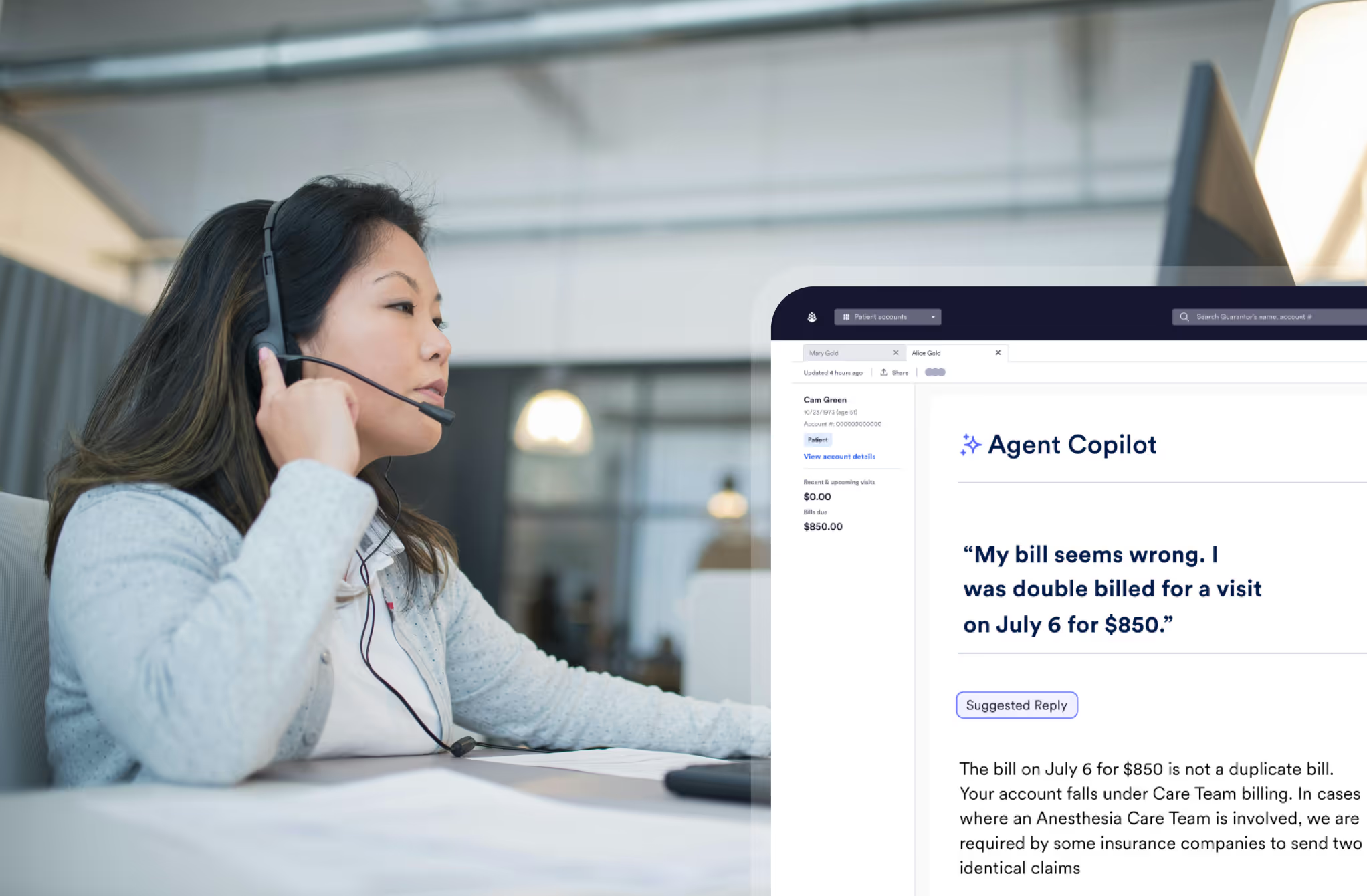
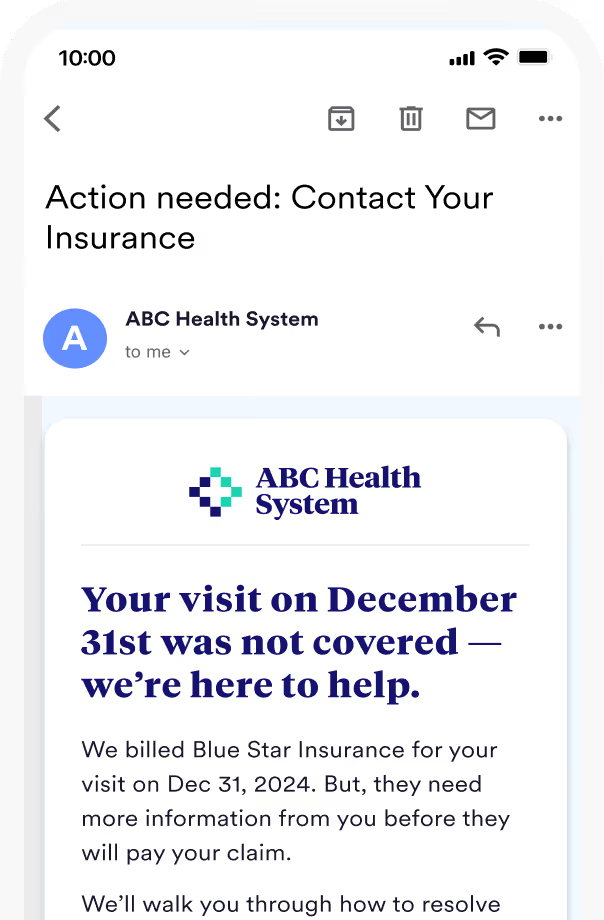
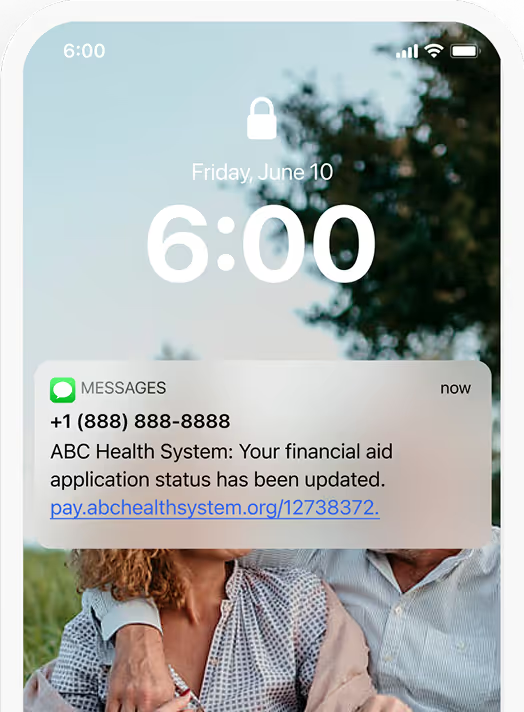
Automate Customer Support
Expect more from your patient financial partner
Accountable Partnership
We go beyond vendor relationships—aligning incentives, co-creating solutions, and evolving with our clients to drive lasting performance.
Complete Platform
By consolidating fragmented tools and workflows, we streamline vendor management and create a more connected patient financial experience.
Data-Driven Optimization
Our platform learns from every interaction, using Cedar Intelligence to continuously refine engagement and deliver better experiences and outcomes.
Results that change lives
We work shoulder-to-shoulder with our partners to help patients access and afford care. But don’t take our word for it.
Our partnership with Cedar will enable our physicians and APCs to continue to prioritize the patient experience with the confidence that Cedar’s best-in-class digital platform will make the back-end process smooth and efficient. We want our patients to have the full spectrum of flexible payment options available to them when paying for medical services.”

Dr. Yogin Patel
CEO, ApolloMD
"We constantly see payments increasing, and Cedar’s communication strategy and user-friendly experience have helped us streamline the end-to-end billing process for patients"
Amanda Six
Vice President of Revenue Cycle, Advanced Dermatology & Cosmetic Surgery
Cedar isn’t just a technology partner—they are a partner. Period. They help us understand what is best-in-class and proactively bring us patient experience best practices, backed by data. Cedar doesn’t just give you the technology and leave you hanging, they’re invested in your success.

Ales Cejka
Vice President of Revenue Cycle Management, Talkiatry
“When you change your outward behavior, patients change theirs. We’re seeing that in patient engagement, patient satisfaction score and the comments they’re leaving. It’s immensely telling.”

Tennille Lizarraga
VP of Revenue Cycle, ApolloMD
“Whenever we hear about Cedar piloting a new tool, we enthusiastically raise our ‘beta partner’ hand. I’m excited about the energy at Cedar, seeing people so passionately engaged. I can’t wait to see what they come up with next!”
Michele Tassone
Sr. Director, Revenue Cycle Services, NAPA
“It’s amazing when you can increase the payment rate by as much as we have AND the patients are happy”

Kelly Black
Vice President RCM, Novant
“I’ve seen what happens when you get the patient financial experience right,” says . “When I came to Unio and saw the same challenges—confused patients, manual processes, stagnant collections—I knew Cedar needed to be part of the solution here too."

Dr. Mike Osmundson
CEO, Unio Health Partners
“LCMC Health is excited to partner with Cedar to empower patients with seamless, transparent and user-friendly financial interactions,” said Greg Feirn, CEO at LCMC Health. “We know it’s imperative to foster positive experiences throughout the entire care journey. Together, we are not just shaping the future of healthcare but ensuring that every aspect of the patient experience, including financial transactions, reflects the high quality of care and convenience our community deserves.”

Greg Feirn
CEO, LCMC Health
“By partnering with Cedar, we’ll be able to streamline and simplify the payment process for all our members—further enhancing their overall experience with Tend, while unlocking new ways for us to elevate engagement.”

Troy Bage
CEO, Tend
"Cedar has shown us that if you make it easy, if you deliver transparency, and if you provide the right information when people need it the most, you can create a remarkable health experience that frees people to be their best.”

Neil Kulkarni
Vice President of Customer and Clinician Experience Solutions, Highmark
“We didn’t have to defend the decision to leadership for months like with other partners, because with Cedar we saw the collections lift almost instantaneously.”

Amy Katnik
COO, ApolloMD
"Cedar gives patients a consistent experience with our brand. Patients are using one system to manage their visits and bills, and these interactions reinforce one another—helping them take the right actions at the right times”

Yesenia Alvarez
Executive Vice President of Operations, Advanced Dermatology & Cosmetic Surgery
“Patient billing is now something I don't worry about on a daily basis. That's how I know it's working.”
Lawanna Johnson
Director of Revenue Cycle, Unio Health Partners
"Due to the seamless integration that USAP and Cedar have set up and clear billing statements provided to patients, there is little confusion among patients about what they owe and why. We hear things like, 'I wish every hospital did it this way,' at least once a month.”

Trish Donohue
Vice President, Shared Services
Cedar understands our patients’ preferences and behaviors, then they leverage this understanding to design a better payment experience. The result is better outcomes for both patients and our business. To me, partnering with Cedar is a no-brainer.”

Todd Yu
CFO, Talkiatry
“After a rocky conversion from three systems to one, Cedar was a breath of fresh air. Everything was smooth and they were hands-on with our vendor, providing exactly what was needed for the data feed. That level of partnership is invaluable.”
Lynn Van Houton
VP, Revenue Cycle Services, NAPA
“I wish all doctors offices would do this!! It makes life so much easier!”
Allegheny Health Network Patient
"Cedar has outperformed every solution we’ve tested in terms of collections and patient experience," says Burns. "At a certain point, it becomes simple math."

Frank Burns
Chief Administrative Officer, USAP
“We recognize the patient experience is so much more than what happens within our walls. By partnering with Cedar, we can give patients an innovative, best-in-class financial experience, ensuring that every part of our system works in coordination to create an effortless care experience for our patients.”

Ric Magnuson
CFO, Allina Health
“I appreciate the ability to pay in installments. This is a blessing to our family.”
Advanced Dermatology & Cosmetic Surgery Patient
Advanced Dermatology & Cosmetic Surgery Patient
Empower the patients others write off
We’ll show you how Cedar can simplify billing, increase coverage, and automate work—delivering stronger margins without added burden on your team.
Thanks for your message!
We will reach back to you as soon as possible.