Earlier today, we announced the launch of the Payer Intelligence Layer (PIL), which is now live for Highmark members who receive care at Allegheny Health Network. We are particularly excited about this announcement because, for us at Cedar, the PIL is more than a product launch. Rather, the PIL unlocks capabilities for providers and payers that simply were not possible until now, and reflects a new orientation to addressing the challenges with patient billing.
The Need for Payer-Provider Collaboration
To understand the significance of the PIL, let’s briefly return to the problem we set out to initially solve. Cedar was founded in 2016 to address the single worst consumer financial experience in the U.S.: paying for healthcare. Our healthcare system drives more consumers to bankruptcy than any other sector. More than half of patient balances after insurance are unpaid, and billing is one of the top drivers of patient dissatisfaction with care events.
For leaders in this space, these challenges are not new. However, to date, these challenges have been framed as a provider problem. Unpaid bills, dissatisfied patients, expensive revenue cycle activities…these are all issues for the provider alone to solve, right?
Wrong. When a provider writes off bad debt as a result of unpaid patient bills, the payer is forced to absorb higher rate increases. When a patient has a bad billing experience, the payer is typically implicated for poor coverage. And, importantly, even when a provider invests in a world-class billing experience that is timely, simple and convenient, it could still be a frustrating experience for the patient if the payer EOB does not match.
Introducing the Payer Intelligence Layer
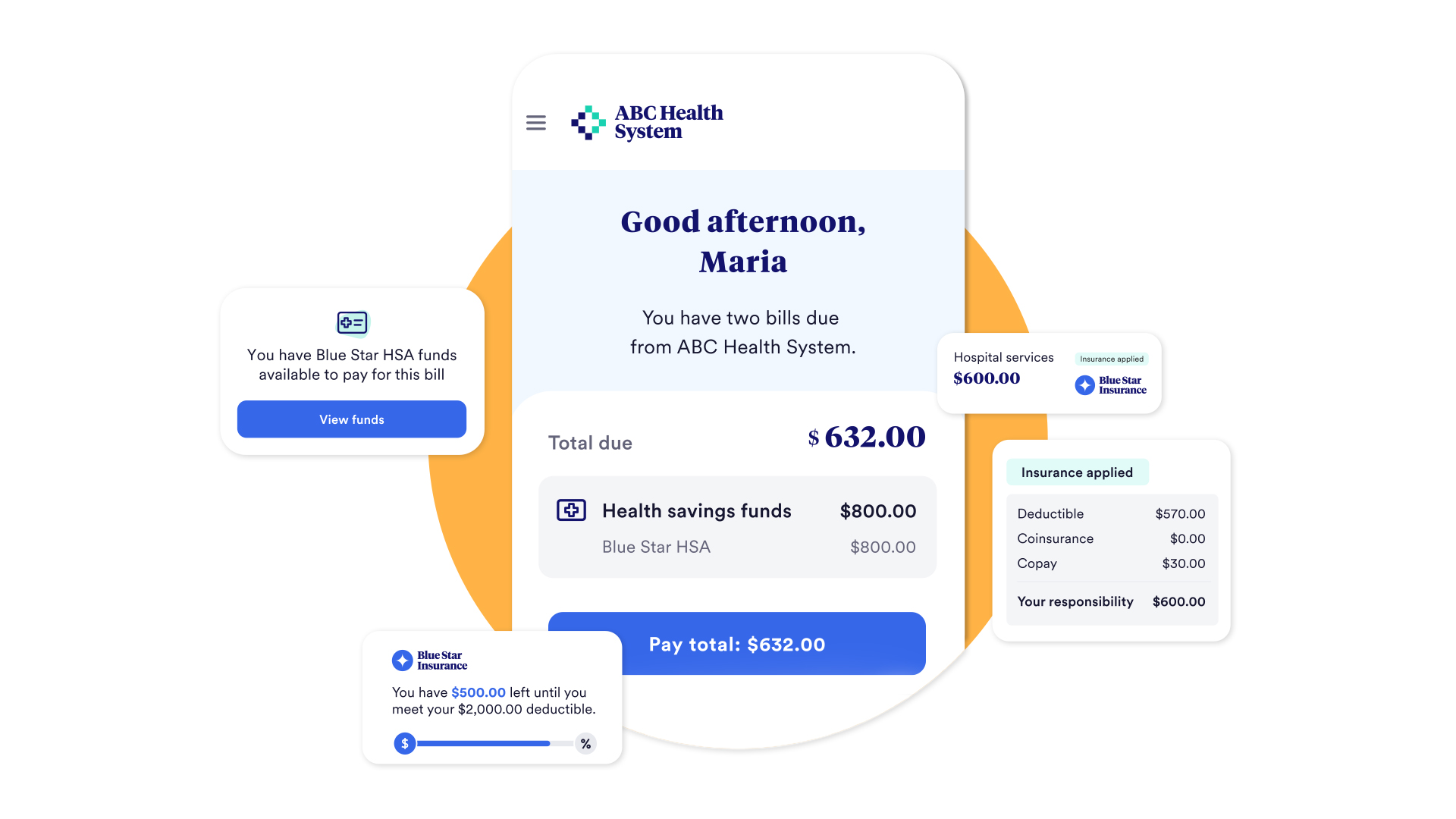
Bottom line: patient billing is a system problem, not a provider problem, and therefore requires a system solution. The PIL is our first step toward introducing a system solution, as we are uniquely incorporating the payer into the provider bill. Specifically, balances due are now matched with EOBs, real-time deductible status is clearly on display and available health account funds are integrated into a smart wallet so that HSA, FSA, HRA dollars are as easy to use as Apple Pay.
Now, the payer and provider are working together to address patient billing challenges. Providers increase patient payments by empowering patients to understand their bills in the context of their benefits, and lower costs by preempting basic questions about benefits coverage before they become inbound phone calls. Payers lower costs by reducing member inquiries about provider bills, and increase both member and provider satisfaction by enabling this uniquely streamlined experience.
Perhaps most importantly, the consumer is no longer stuck in the middle of the payer and provider when trying to resolve a billing question. Instead of calling in for help or logging into multiple portals, consumers get clarity and gain confidence with a single source of information to manage and resolve healthcare bills.
What’s Next: Connecting the Healthcare Ecosystem
Integrating the payer is the first step in our broader strategy towards ecosystem connectivity. For a single hospital encounter, consumers might have to navigate multiple, siloed interactions beyond the payer and provider: HSA bank, Medicaid enrollment vendor, financing underwriter, and affiliated physician bills, to name a few. The result: a mess of paperwork that leads to confusion, missed payments, administrative waste and serious financial ramifications for all parties involved. We are excited—and committed—to align the ecosystem around delivering a truly transformational consumer financial experience in healthcare.
For too long we have placed the burden of billing on providers alone. Given the number of stakeholders that “touch” the consumer along the end-to-end financial journey, it is not surprising that efforts to address the patient billing challenge through the lens of just one provider—or one set of EMR tools—ultimately fall short. With the launch of PIL, we are excited to introduce a new, system approach to what is inevitably a system problem.
Seth Cohen is President of Cedar.